No products added!
Written by
admin
June 20, 2024
Scars on the skin
Before we tell you more about scars, it is first important to learn a little more about the skin. What many people do not know is that the skin is the largest organ of the human body and covers an area of 1.5 to 2 square meters in adults.
The skin consists of 3 different layers:
- The epidermis, or epidermis, forms the top layer of the skin. This outer layer of skin provides protection and firmness. This skin layer is continuously renewing!
- The dermis is the middle layer that provides further firmness to the skin. This layer contains the hair roots, nerves, blood vessels and sebaceous and sweat glands. The epidermis and dermis together form the ‘cutis’ or “skin”.
- The bottom layer of the skin, the subdermis, or subcutis consists mainly of fat, collagen tissue and blood vessels. This is the separating layer between skin and muscles/tendons and is the protective layer for the organs that lie beneath this layer.

The skin barrier: the waterproof outer boundary of your body that holds the upper layers of your skin together!.
The epidermis layer also consists of two layers. The top layer of the epidermis, or the stratum corneum, ensures the barrier function of the skin. This function makes it possible to keep irritating substances, such as viruses and bacteria, out and to keep moisture within the body. The second layer, the mucus layer, lies directly beneath the stratum corneum and ensures a continuous growth of new cells that replace the damaged or dead stratum corneum cells. A beautiful process that continues throughout your life!
If the skin and therefore the barrier are damaged, moisture cannot be retained and the skin may become sensitive.
You can recognize sensitive skin by itching and/or roughness, dryness and red skin. In addition, the skin may feel burning, stinging or pulling. Damage to the skin barrier occurs, among other things, in scars, stretch marks and burns.
“You can recognize sensitive skin by itching and/or roughness, dryness and red skin.”
Functions of the skin
The skin has several functions. We describe four of the important functions of the skin below:
- The skin provides protection and provides a physical barrier against injuries, UV rays, bacteria and viruses;
- The skin is an important sense. Due to the tactile nerves with ends in the dermis, it is possible to experience pain, heat, cold and pressure;
- The skin has a very important heat regulation function. The skin enables the body to deal with heat fluctuations in the environment;
- The skin produces vitamin D. By absorbing UV rays, the skin produces Vitamin D.
What is a scar?
A scar is the reaction of the skin to damage caused, for example, by a (severe) burn or a medical or cosmetic procedure.
When the skin is severely damaged, for example in the form of a wound, the body has the ability to repair this damage immediately
 Promotes healing
Promotes healing
 Keep the skin supple
Keep the skin supple
 Promotes healing
Promotes healing Keep the skin supple
Keep the skin supple
This beautiful process or wound healing consists of the following four phases:
- Phase 1, blood clotting : when the wound is still open, fibrin (a blood clotting protein) is produced to cover the wound as quickly as possible. A scab forms on the wound, which is actually a net of threads to which proteins, blood cells and platelets stick;
- Phase 2, inflammation : Dilation of the blood vessels allows blood cells, proteins and water to enter the wound. The skin turns red and swells, often combined with a burning sensation;
- Phase 3, regeneration: From the edges of the scar, the skin will start to grow inward again because blood vessels and collagen are produced. This beautiful process ensures closure of the wound;
- Phase 4, maturation . When the wound has closed and the crust is gone, a red (small superficial blood vessels) and raised scar will appear. Over time this will fade into a quiet, white and non-raised scar. The redness disappears because the superficial blood vessels gradually disappear and a white skin structure develops. The so-called maturing of a scar can take a longer period, this of course depends on the shape, size and location of the injury.

How does a scar form and what are the possible complaints?
When will I get a scar?
If the deeper layers of the skin are damaged, such as a surgical wound or second-degree or third-degree burn, a visible scar is created.
If damage/injury is limited to the epidermis, the skin has the ability to heal itself without a visible scar. These superficial injuries occur with abrasions or first-degree burns. Proper care of the scar produces good results.
Possible complaints of a scar
When a scar is damaged, the skin barrier is damaged. This means moisture is not retained in the skin. Due to the loss of moisture, the skin can become sensitive and show the following signs:
- Dryness
- Redness
- Itch
- Roughness
- A burning, stinging or pulling sensation on the skin
“ After closing the skin, the 'normal' scar is often red, minimally raised above the skin and can possibly cause complaints”
What types of scars are there?
There are several types of scars that form after (severe) skin damage:
- The ‘normal’ scar . After the skin has been closed, a fresh, normal scar is often red, minimally raised above the skin and may cause complaints. Over time, the scar shrinks and the symptoms disappear. This maturation process can take several weeks to one or two years. Recovery obviously depends on the size, severity and location of the injury. The longer the recovery from the injury takes, the greater the chance of scarring. Any symptoms of the scar may return after the scar has matured due to the influence of cold weather or UV rays;
- The hypertrophic scar. The hypertrophic scar is a red, tender, raised scar that has grown within the margins of the original lesion. The exact reason for the development of a hypertrophic scar is not known. It is thought that the pressure on the scar, the location of the injury, patient age, gender and skin color have an influence. It usually takes a few months for a hypertrophic scar to develop. Once the stable phase – during which the scar becomes less sensitive – has begun, the elevation and redness will decrease.
- Keloid scar. One will see a very raised scar which, unlike a hypertrophic scar, will grow and sometimes proliferate beyond the edges of the original wound. The skin is not able to repair the injury in a normal way and it is not possible to form a normal scar. There is also no clear explanation for the development of this type of scars. It has been proven that patients with a dark skin color are more likely to develop a keloid scar.
- Atrophic scar. An atrophic scar is a type of scar that widens over time and lies deeper in the skin. Because there is a disruption in the healing process, there is less scar tissue present and the scar lacks thickness. Causes can be excessive tension or pressure on the wound or poor blood circulation in the wound. Radiation and medication are also seen as causes.
- When a scar contracts, the skin can become shorter and less stretchy. This can cause curvature or restriction of movement of, for example, a finger. Scars that occur in growing children can cause such a situation. To give these scars more space, multiple operations are often necessary.
What is the best way to treat a scar?
It is very important to care for the injury/wound as best as possible and then keep it clean. After closing the wound and/or removing the stitches, treatment of the fresh scar can begin. There are several ways to treat this scar:
- Topical treatment with scar creams, silicone plasters and gels;
- Applying pressure bandages, wearing pressure clothing;
- Laser and radiotherapy;
- Peelings and injections with corticosteroids: these are forms that are used for large scars or scars that are restless, such as hypertrophic or keloid scars.
Ultimately, a scar is a newly formed protective layer on top of the underlying tissue. This new layer lacks most of the properties of the ‘old’ skin. This new tissue has no natural fat layer, is more difficult to absorb nutrients and is less easy to hydrate.
Common complaints are cracks and fissures in the scar because it simply lacks the standard skin properties. The result of these complaints is a restless scar with a longer healing process. These cracks/fissures are also visible in growing children, because the scar stretches as the child grows.
It is therefore important to permanently hydrate the skin, so that a calm situation is created, without excessive tension.
Once a scar has matured, using a scar cream is no longer useful and is therefore not recommended. When the scar becomes sensitive or restless, for example due to the effects of the weather, the moisturizing effect of a scar cream is useful.
“Silicone forms a semi-permeable (permeable), protective layer on the scar and thus prevents moisture loss from the skin”
International guidelines
According to international guidelines for the treatment of scars, sunlight should be avoided, because the influence of UV rays can cause the scar to become restless. In addition, a topical treatment – in the form of a scar cream – is preferred. Surgical interventions or other forms of treatment are only used if recovery is problematic or if it becomes a hypertrophic or keloid scar.
Our advice:
- Care for injuries and/or wounds : it is important to keep the wound area clean and well cared for. Possible infections in the wound area can lead to a delayed recovery and thus a difficult formation and therefore a restless scar
- Always avoid UV rays : it is essential to avoid sunlight because of its effect on the scar in terms of shape, complaints and discoloration. The skin can discolour due to the formation of pigment. Pigmentation of the scar cannot be reversed and is permanent;
- We recommend that you remain patient: sometimes a scar takes a long time to mature, especially after a larger or deeper injury to the skin.
- Always make sure you have a good scar cream : it makes sense to support skin recovery with a good scar cream. Scar creams based on silicone supplemented with active ingredients are preferred.
The main ingredients of Staudt® scar cream are:
- Silicone forms a semi-permeable (permeable), protective layer on the scar and thus prevents moisture loss from the skin. An important property of silicone is to inhibit the growth of scar tissue, which can flatten a scar;
- Betaglucan strengthens the skin’s own immune system and promotes skin recovery;
- Bisabolol soothes, stimulates the wound healing process and has an anti-inflammatory effect;
- Hyaluronic acid ensures better moisture absorption, prevents moisture loss and helps maintain the elasticity of the skin;
- Honey has an antibacterial effect. Prebiotic fibers protect against irritants and also strengthen the skin;
- Natural oils have a soothing and nourishing effect on the skin.
Do I now use SPF 30 or SPF 50 to protect my scar against sunlight?
According to international guidelines for the treatment of scars, sunlight should be avoided, because the influence of UV rays can cause the scar to become restless. It is therefore important to avoid the sun if you have a (fresh) scar, but that is not always possible.
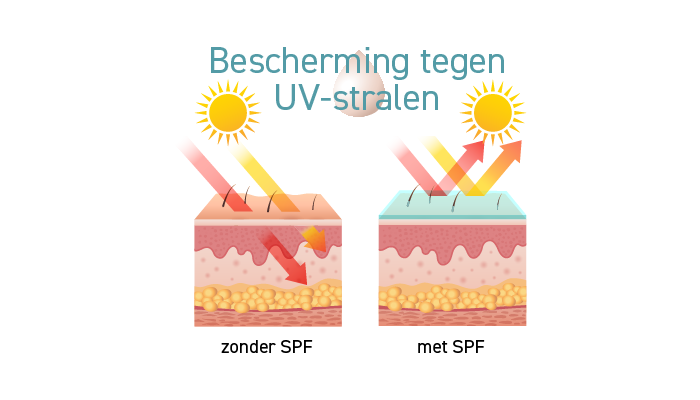
Logically, it is therefore important to use a good scar cream with a Sun Protection Factor (SPF) of at least 30. The SPF value of a sunscreen indicates how well your skin is protected against UVB rays.
Despite many recommendations from manufacturers, various scientific studies have shown that a higher SPF does not lead to much greater protection of the skin (scar):
- SPF 30 blocks 96.7% of all UVB rays
- SPF 50 blocks 98% of all UVB rays
The conclusion is that the SPF 50 provides 1.3% extra protection against sunlight
There is therefore little difference in the protection level of SPF 30 compared to SPF 50, making SPF 30 suitable for the scar.